ELMIRON LITIGATION: EMERGING TORTS
By Rachel Shkolnik,
Hunter J. Shkolnik
Napoli Shkolnik, PLLC
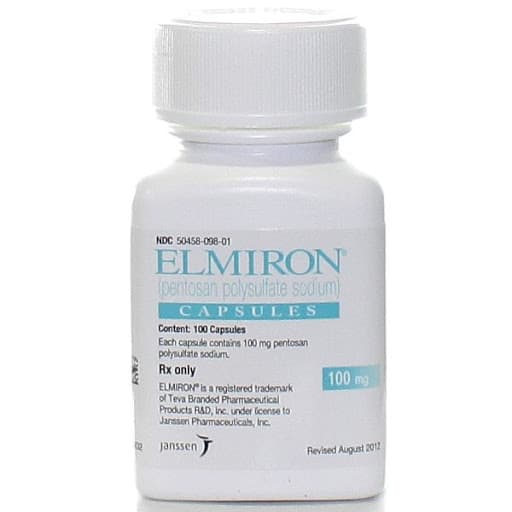
(May 27, 2020) The nationwide Elmiron eye damage litigation has picked up headlines over the past several months. Elmiron, the brand name for pentosan polysulfate sodium, is a semi-synthetically produced heparin-like macromolecular carbohydrate derivative.[1] The lawsuit is centralized around the basis that the drug causes an eye disorder called maculopathy and other disorders of the retina that may lead to blindness. The lawsuits underlying claim is based on failing to properly warn the public about the risk of vision problems.[2]
Interstitial Cystitis
Elmiron is prescribed to treat interstitial cystitis indicated for the relief of bladder pain or discomfort associated with a bladder condition interstitial cystitis (IC).[3] IC, also known as painful bladder syndrome, is a chronic bladder condition in which individuals are symptomatic of bladder or pelvic pain, urinary frequency, urgency and nocturia. IC is known to affect more woman than men. The American Urological Association (AUA) established IC treatment guidelines separating into six tiers of increasing invasive therapy.[4] Elmiron is not a first-line treatment for IC.
These treatment guidelines begin with the simple lifestyle changes and progress to levels that are more invasive.[5] AUA recommends second-line treatment of IC to incorporate multi-modal pain management approaches including manual therapy and oral therapy options such as pentosyn polysulfate (Elmiron).[6] Elmiron is not the best nor the only option for treating interstitial cystitis.
[2] https://www.drugwatch.com/elmiron/lawsuits/
[3] https://www.orthoelmiron.com/sites/www.orthoelmiron.com/files/021906-150224.pdf
[4] Colaco M, Evans R. Current guidelines in the management of interstitial cystitis. Transl Androl Urol. 2015;4(6):677‐683. doi:10.3978/j.issn.2223-4683.2015.11.03
[5] Colaco M, Evans R. Current guidelines in the management of interstitial cystitis. Transl Androl Urol. 2015;4(6):677‐683. doi:10.3978/j.issn.2223-4683.2015.11.03
The Injury
Elmiron’s associated eye disease is called pigmentary maculopathy. The signature Elmiron eye disease is affecting the central part of the retina. It is caused by retinal toxicity or drug-induced toxicity that damages the retina. Pigmentary maculopathy occurs when the pigment cells alter in the retina causing significant eye damage and vision loss while often changing the eye color.[7] Pigmentary maculopathy symptoms include central visual loss, dark spots in the visual field, prolonged dark adaptation lighting issues, distorted lines, muted colors, and change in eye color.[8] Pigmentary maculopathy may be mild or severe depending on the amount of retinal damage that has occurred.[9]
The macula is the part of the retina that is responsible for producing accurate and highly sensitive vision. Maculopathy, also known as macular degeneration, is a disease related to the central part of the retina, called macula. Maculopathy is characterized by a progressive loss of central vision, usually bilateral, that greatly impairs vision functions. There are several types of maculopathy. Not all maculopathy’s are caused by retinal toxicity.
People who suffer from eye conditions are being misdiagnosed because their symptoms are similar to macular degeneration or even macular pattern dystrophy. Age-related conditions like macular degeneration don’t appear until around age 60. Macular pattern dystrophy stems from genetics. People may have an Elmiron related injury when they are suffering from eye damage such as: blurred vision, central vision loss, trouble reading, trouble adjusting to dim lighting, prolonged dark adaptation/poor light to dark adaptation, glare, blind spots, metamorphopsia, and blindness.
Dry maculopathy is more frequent compared to wet maculopathy. In 90% of maculopathies are dry ones: the retina gets thinner because vision cells stop working and disappear; for this form, also known as atrophic maculopathy, laser therapy has proven to be ineffective. Nutritive factors transport and waste elimination by the retinal pigmented epithelium (RPE) are slowed down: yellowish intra-retinal deposits (drusen) or pigmented (dystrophy, focal pigment) appear. There is usually a small vision impairment and only in a few cases have been experienced atrophied zones that look like retinal stretch marks and also involve the central part (fovea).
A client might have several conditions resulting in eye sight loss which may or may not be Elmiron related. A person with macular degeneration, which is damage to the macula area in the retina, will suffer from central visual loss, dark spots in the visual field, dark lighting issues, distorted lines, and muted colors. An individual with diabetic retinopathy, which is damage to the blood vessels in the retina, will suffer from blind spots, dark spots and streaks in the visual field, dark lighting issues, and muted colors. An individual with glaucoma, which is damage to the optic nerve in an eye, will suffer from general visual loss, glare and halos in the visual field, dark lighting issues, and redness in the eye. An person with cataracts, which is clouding of the lens of the eye, will suffer from general visual loss, halo and glare in the visual field, dark lighting issues, and whitening in the pupil.
Several eye diseases have similar symptoms to Elmiron induced injuries. Thus, it is vital to obtain fundus and OTC imagining to detect diseased regions and/or atrophy in areas of the retina. Fundus imagery involves photographing the interior surface of the eye to record color images of the condition of the interior surface of the eye, in order to document the presence of disorders and monitor their change over time. The retina is imaged to document conditions such as pigmentation maculopathy, diabetic retinopathy, age related macular degeneration, macular edema and retinal detachment.
[6] Colaco M, Evans R. Current guidelines in the management of interstitial cystitis. Transl Androl Urol. 2015;4(6):677‐683. doi:10.3978/j.issn.2223-4683.2015.11.03
[7] https://www.livescience.com/34781-macular-degeneration-eye-disease.html
[8] https://www.livescience.com/34781-macular-degeneration-eye-disease.html
[9] https://www.livescience.com/34781-macular-degeneration-eye-disease.html
Literature
Numerous studies conducted by doctors from highly respected hospitals and universities have found a possible connection with long term Elmiron use and severe eyes disorders that can lead to blindness. Peer reviewed literature has established a causal connection between Elmiron and pigmentary maculopathy. Pigmentary maculopathy may render patients with severe central vision loss that is not repairable or operable. Literature supports not only a dose and duration association, but latency based on load effect due to the deposit of molecules in the RPE within the macula.
In May 2018, Emory Eye Center conducted a case study of six adult patients who were treating IC with pentosan polysulfate sodium. The doctors began noticing a new eye disease deemed pigmentary maculopathy in patients with long term Elmiron.
In April 2019, the Emory Eye Center did a further case study of ten patients. The doctors reported that over the last four years, patients who did not treat IC with pentosane polysulfide sodium were not experiencing pigmentary maculopathy.
The first clinical population based study came from Kaiser Permanente in 2019. Kaiser Permanente conducted a study based of 4.3 million patients. Patients showed clear evidence of this specific maculopathy, which was believe was associated with PPS exposure. The research was presented at the “AAO 2019”—the annual meeting of the American Academy of Ophthalmology at Moscone Center, San Francisco. The study revealed that eye damage increased with the quantity of Elmiron intake.[10]
[10] https://www.sciencedirect.com/science/article/abs/pii/S0161642020300403
A Harvard case study involved examining a female with a history of eighteen years of Elmiron use at a low dose of 200mg/day. She was initially presented with symptoms that included blurry vision, difficulty seeing at night, and pigmentary changes in the retina. Two years into the study she returned with more extensive eye damage consistent with pigmentary maculopathy. Harvard doctors concluded that long term Elmiron use results in progression of the disease even after cessation of Elmiron.
Furthermore, animal studies confirm that there is detrimental retinal effects found in mice as a result of pentosan polysulfate administration.
Label: No Warnings!
Since the original report, there have been more than a dozen papers published in the medical literature regarding the atypical maculopathy associated with Elmiron use. Despite all the reports, the label and prescribing information that accompany Elmiron when prescribed to patients contains the following: “Warnings: None.” Elmiron provides no education about potential vision changes nor instruction to have annual eye exams despite the fact that the label has been changed at least four times.
The Elmiron label has been updated several times, but at no time has it contained any information about visual loss, including pigmentary maculopathy, in any section of the label. The drug makers did not do anything to warm the eye damage risks associated with Elmiron- no voluntary recall, no warning label added to the box, not even an announcement to conduct further investigation.
In October 2019, Health Canada announced pigmentary maculopathy would be added to the “warnings and precautions,” “post – market adverse drug reactions” and “consumer information” sections of the Canadian monograph. However, the United States label still did not change the label.
Client demographics
The studies suggested the client demographics involve mostly woman between the ages of thirty-seven and seventy-nine years.[11] Elmiron intake lasts as little as three years and as long as twenty-two years.[12] Common presenting symptoms include: blurred vision, prolonged dark adaptation, and metamorphopsia (which is a type of distorted vision in which a grid of straight lines appears wavy and parts of the grid may appear blank).[13] The visual symptoms last from one to nine years. The visual acuity, which is an ability to discern the shapes and details of the things, ranged from 20/20 to 20/300 in the right eye, and ranged from 20/15 to 20/400 in the left eye.[14]
[11] Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Med. 2014;175(4):30-37; Vora R, Patel A, Melles RS. Maculopathy associated with pentosan polysulfate therapy: the KPNC experience. Paper presented at: AAO Retina Subspecialty Day; October 12-13, 2019; San Francisco, CA.
[12] Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Med. 2014;175(4):30-37; Vora R, Patel A, Melles RS. Maculopathy associated with pentosan polysulfate therapy: the KPNC experience. Paper presented at: AAO Retina Subspecialty Day; October 12-13, 2019; San Francisco, CA.
Who is responsible?
As indicated on the label, Elmiron® is a Registered Trademark of Teva Branded Pharmaceutical Products R&D, Inc. under license to Janssen Pharmaceuticals, Inc. On September 26, 1996, the U.S. Food and Drug Administration (FDA) approved Elmiron. From approximately August 2002 until August 2004, Janssen Research & Development LLC held the NDA for Elmiron. From July 2004 until August 2008, Janssen Pharma, Ortho-Mcneil Pharmaceuticals, INC. held the NDA for Elmiron. Since August 2008, Janssen Pharmaceuticals, INC., is the current U.S. Food and Drug Administration (FDA) New Drug Application (NDA) who now manufactures and distributes Elmiron.
Makers of generic drugs cannot be sued for not warning patients of the drugs’ dangerous side effects. However, this issue is not present in the Elmiron litigation, because there is no therapeutically equivalent version of Elmiron available in the United States. The litigation is only involves brand named drugs.
Pending lawsuits
There are multiple Elmiron suits pending in court. On March 26, 2020, the first lawsuit was brought against Teva Branded Pharmaceutical Products R&D, Teva Pharmaceuticals USA, Inc., Janssen Pharmaceuticals, Inc, and Johnson & Johnson, Inc. in the United States District Court for the District of Connecticut. The suit alleges three counts under the Connecticut Products Liability Act.
Shortly thereafter a lawsuit was brought against Janssen Pharmaceuticals, INC., f/k/a Ortho-McNeil-Janssen Pharmaceuticals, Inc., f/k/a Janssen Pharmaceutica Inc.; Ortho-Mcneil Pharmaceuticals, Inc.; Janssen Research & Development LLC f/k/a Johnson & Johnson Research & Development, L.L.C.; Janssen Ortho LLC; and Johnson & Johnson in the Middle District of Florida with six counts. As of now, there is no multi district litigation involving Elmiron but one would expect a filing for such will be coming in the near future.
[13] Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Med. 2014;175(4):30-37; Vora R, Patel A, Melles RS. Maculopathy associated with pentosan polysulfate therapy: the KPNC experience. Paper presented at: AAO Retina Subspecialty Day; October 12-13, 2019; San Francisco, CA.
[14] Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Med. 2014;175(4):30-37; Vora R, Patel A, Melles RS. Maculopathy associated with pentosan polysulfate therapy: the KPNC experience. Paper presented at: AAO Retina Subspecialty Day; October 12-13, 2019; San Francisco, CA.
For additional Elmiron information from Napoli Shkolnik, PLLC see: https://www.napolilaw.com/practice-areas/pharmaceutical-litigation/national-elmiron-eye-disease-lawyers/
Case Criteria
A typical Elmiron claim involves woman, between the ages of thirty to sixty years, ingested Elmiron for at least one year, the Elmiron dosage is at least hundred mg, and suffers from one of the qualifying injuries. The qualifying injuries include: pigmentation maculopathy, pigmentation macular degeneration, pigmentation maculitis, retinal maculopathy or dry macular degeneration. A person may have a viable claim if they have at least four years of Elmiron use with contemporaneous qualifying symptoms such as blurred vision, central vision loss, or prolonged light adaption.
Although not common, men might have a viable claim if they fall under the criteria. There have been several FDA adverse events reports by men would fall under the case criteria.
Lastly, as in all drug related product liability cases it is important to consider alternative causation issues. Lawyers should keep an eye out for clients with severe kidney disease; liver disease; tamoxifen use; and pre-existing retinal disease as these may affect the viability of claims. Moreover, with the current Covid 19 pandemic and the political debate surrounding the use of Hydroxychloroquine as an off-label treatment for the virus, we expect to see increasing numbers of macular degeneration cases unrelated to Elmiron use and these clients should be screened closely.

About the author: https://www.napolilaw.com/napoli-attorney/rachel-l-shkolnik/
(212) 397-1000 Ext. 1050 | [email protected]
360 Lexington Avenue, Eleventh Floor, New York, NY 10017
vCard-R. Shkolnik

Hunter J. Shkolnik
360 Lexington Avenue, Eleventh Floor, New York, NY 10017
For additional Elmiron information from Napoli Shkolnik, PLLC see: https://www.napolilaw.com/practice-areas/pharmaceutical-litigation/national-elmiron-eye-disease-lawyers/




Comments